Brer Insurer and the briar patch

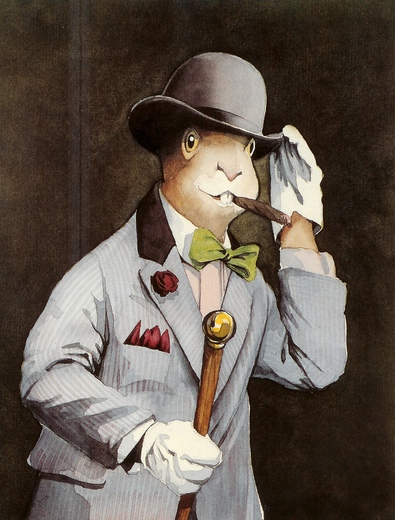
(Illustration from the Wrens Nest Blog, part of the Joel Chandler Harris historical site in Atlanta's West End.)
The story looks at two vendors, UnitedHealth and McKesson. It notes both are upgrading their IT capabilities and spending big to make required changes.
The idea is that this is all some regulatory hassle, a concession they are being forced to make by politicians, and that they will now compete to provide these capabilities to their brethren.
Uh, no.
- This is not some new regulatory burden being imposed on them by a cruel and corrupt Administration. It is the greatest opportunity the health insurance industry has ever had, and was crafted mainly by its lobbyists.
- UnitedHealth and McKesson are not going to be bringing these changes to their brethren. No insurer wants to be dependent on a rival, and McKesson's focus is on the hospital market, not insurance.
- What's missing from the story is the opportunity this spells for companies like IBM, which has already signed on Aetna to its new cloud offering.
As I have noted here before, the main feature of health reform is to turn economic incentives on their head. Insurers can't cover only the healthy now, they also have to cover the sick. The market pressure they can apply moves from the buyers to the sellers of health services.
UnitedHealth has responded by buying up every vendor it can find in this space, through its Ingenix unit, and is cobbling together a solution that will bind clinics and hospitals to it, based on rigid cost controls Ingenix will integrate. Aetna is depending on IBM. Kaiser has its own IT department.
Other insurers also have IT departments, like Kaiser, but they may face problems grabbing hold of the new opportunities. Opportunities like wellness services, like managing best practices, and requiring physicians to use comparative effectiveness studies if they want to stay on their networks.
This is a huge opportunity for companies like HP (through EDS), like Dell (through Perot Systems), like Microsoft (through Amalga) and for Oracle. Just as it is for IBM, which has already shown its hand. It's one way mainstream IT vendors are going to gobble up the specialists.
Tomorrow's health insurance profits depend on cutting the cost of care, limiting the spread of chronic conditions, and maintaining discipline among network physicians. If it's a regulatory burden, it's one the industry sought out.
It is, to return to Mr. Harris, who wrote his "Uncle Remus Stories" from tales told by black slaves in the 19th century, Brer Rabbit's briar patch.